HEALTHCARE COST AND UTILIZATION PROJECT – HCUP
A FEDERAL-STATE-INDUSTRY PARTNERSHIP IN HEALTH DATA
Sponsored by the Agency for Healthcare Research and Quality
INTRODUCTION TO
THE HCUP NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS)
2020
|
These pages provide only an introduction to the 2020 NASS. For full documentation and notification of changes, visit the HCUP User Support (HCUP-US) website at www.hcup-us.ahrq.gov. |
Issued November 2022
Agency for Healthcare Research and Quality
Healthcare Cost and Utilization Project (HCUP)
5600 Fishers Lane
Mail Stop 7W25B
Rockville, MD 20857
NASS Data and Documentation Distributed through the HCUP Central Distributor:
Website: www.hcup-us.ahrq.gov
Phone: (866) 290-4287 (toll free in the United States)
Email: hcup@ahrq.gov
Table of Contents
INDEX OF TABLES
INDEX OF FIGURES
HCUP NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS)
|
|
***** REMINDER ***** |
All users of the NASS must take the online HCUP Data Use Agreement (DUA) training course and read and sign a Data Use Agreement. Details and links may be found on the following page. Authorized users of HCUP data agree to the following restrictionsa:
Any violation of the limitations in the Data Use Agreement is punishable under Federal law by a fine, up to five years in prison, or both. Violations may also be subject to penalties under State statutes. |
a This is a summary of key terms of the Data Use Agreement for Nationwide Databases; please refer to the DUA for full terms and conditions. |
HCUP DATA USE AGREEMENT REQUIREMENTS
All Healthcare Cost and Utilization Project (HCUP) data users, including data purchasers and collaborators, must complete the online HCUP Data Use Agreement (DUA) Training Course and read and sign the HCUP DUA. Proof of training completion and signed DUAs must be submitted to the HCUP Central Distributor.
Data purchasers will be required to provide their DUA training completion code and will execute their DUAs electronically as a part of the online ordering process. The DUAs and training certificates for collaborators and others with access to HCUP data should be submitted directly to the HCUP Central Distributor using the contact information below.
The online DUA Training course is available at www.hcup-us.ahrq.gov/tech_assist/dua.jsp.
The HCUP Nationwide DUA is available on the HCUP User Support (HCUP-US) website at www.hcup-us.ahrq.gov
HCUP CONTACT INFORMATION
HCUP Central Distributor and HCUP User Support
Information about the content of the HCUP databases is available on the HCUP User Support (HCUP-US) website (www.hcup-us.ahrq.gov).
If you have questions, please review the HCUP Frequently Asked Questions located at www.hcup-us.ahrq.gov/tech_assist/faq.jsp.
If you need further technical assistance, please contact the HCUP Central Distributor and User Support team at:
Phone: (866) 290-HCUP (4287) (toll free in the United States)
Email: hcup@ahrq.gov
Fax: (805) 792-5313
Mailing address:
HCUP Central Distributor
c/o IBM
5425 Hollister Ave, Suite 140
Santa Barbara, CA 93111
We would like to receive your feedback on the HCUP data products. Please send user feedback to hcup@ahrq.gov.
|
WHAT IS THE NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS) |
|
|
WHAT'S NEW IN THE 2020 NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS) AND LOAD PROGRAMS? |
|
|
UNDERSTANDING THE NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS) |
|
HEALTHCARE COST AND UTILIZATION PROJECT — HCUP
A FEDERAL-STATE-INDUSTRY PARTNERSHIP IN HEALTH DATA
Sponsored by the Agency for Healthcare Research and Quality
HCUP Nationwide Ambulatory Surgery Sample (NASS)
ABSTRACT
The Nationwide Ambulatory Surgery Sample (NASS) is part of the Healthcare Cost and Utilization Project (HCUP), which is sponsored by the Agency for Healthcare Research and Quality (AHRQ).
The NASS was created to enable analyses of selected ambulatory surgery utilization patterns and to support public health professionals, administrators, policymakers, and clinicians in their decision making regarding this critical source of care. The NASS contains clinical and resource-use information that is included in a typical hospital-owned facility record abstract, including patient characteristics, clinical diagnostic and surgical procedure codes, disposition of patients, total charges, expected source of payment, and facility characteristics. Therefore, it enables government entities, industry professionals, and researchers to develop research concepts with data-driven applications.
The NASS is the largest all-payer ambulatory surgery database that has been constructed in the United States, yielding national estimates of selected therapeutic ambulatory surgery encounters performed in hospital-owned facilities. The ambulatory surgeries selected for inclusion in the NASS are therapeutic procedures which require the use of an operating room, penetrate or break the skin, and involve regional anesthesia, general anesthesia, or sedation to control pain. To be considered in-scope for the NASS, ambulatory surgeries are also required to have a relatively high annual volume or aggregate total facility charge. Examples include ambulatory surgeries such as cataract surgery, appendectomy, gastric bypass, hysterectomy, hernia repair, spinal fusion, and hip replacement.
The NASS contains information from 7.8 million ambulatory surgery encounters at 2,899 hospital-owned facilities that approximate an estimated 67 percent stratified sample of U.S. hospital-owned facilities performing ambulatory surgeries. Weights are provided to calculate national estimates totaling 10.3 million ambulatory surgery encounters in 2020.
The NASS is drawn from statewide data organizations that provide HCUP with data from ambulatory surgery encounters. Thirty-five HCUP Partner organizations participated in the 2020 NASS (Appendix A, Table A.1)
By stratifying on important facility characteristics, the NASS is designed to be representative of U.S. hospital-owned facilities that perform ambulatory surgeries. Post-stratification for the purposes of weighting is based on the following characteristics:
Access to the NASS is open to users who sign Data Use Agreements. Uses are limited to research and aggregate statistical reporting.
For more information on the NASS, visit the AHRQ-sponsored HCUP User Support (HCUP-US) website at www.hcup-us.ahrq.gov/db/nation/nass/nassdbdocumentation.jsp.
INTRODUCTION TO THE NATIONWIDE AMBULATORY SURGERY SAMPLE (NASS)
1. OVERVIEW OF NASS DATA
The Healthcare Cost and Utilization Project (HCUP) Nationwide Ambulatory Surgery Sample (NASS) was created to enable analysis of selected ambulatory surgery utilization patterns and to support public health professionals, administrators, policymakers, and clinicians in their decision making regarding this critical source of care. The NASS has many research, policy, and other data-driven applications because it contains clinical and nonclinical information about in-scope ambulatory surgeries and diagnoses as well as geographic, facility, and patient characteristics.
1.1 NASS Data Sources, Hospitals, and Encounters
The 2020 NASS is sampled from the HCUP State Ambulatory Surgery and Services Databases (SASD). The SASD include various types of outpatient services, such as observation stays, lithotripsy, radiation therapy, imaging, chemotherapy, and labor and delivery. The specific types of ambulatory surgeries and outpatient services included in each SASD vary by State and data year. All SASD include data on ambulatory surgery encounters from hospital-owned facilities. Some States include data from nonhospital-owned facilities, although these are not included in the NASS1. The SASD do not include ambulatory surgery encounters that were subsequently admitted to the same hospital for inpatient care. As such, the NASS does not contain any encounters admitted to the inpatient setting from the ambulatory setting. Information on patients admitted to the hospital following ambulatory surgery is included in the HCUP State Inpatient Databases (SID).
Note that in data year 2019, the NASS was sampled from the SASD and State Emergency Department Databases (SEDD) because analyses revealed additional encounters involving "narrow" or in-scope surgeries that were started in the emergency department and appeared in the SEDD but not in the SASD. As a result, these emergent ambulatory surgeries are undercounted in the 2016–2018 NASS. The procedures most impacted by this issue include appendectomy and removal of ectopic pregnancy (each undercounted by more than 50%) and cholecystectomy (undercounted by approximately 10%). Starting with data year 2020, records containing emergent in-scope ambulatory surgeries appear in both the SASD and SEDD (if a State provides both data types). As such, only the SASD are required for the 2020 NASS sample.
The number of States, hospital-owned facilities, and ambulatory surgery encounters in the NASS varies by year (Table 1).
Table 1. Number of States, Hospital-Owned Facilities, and Encounters in the NASS by Year
| Data Year | States in the NASS | Number of Hospital-Owned Facilities | Number of AS Encounters, Unweighted | Number of AS Encounters, Weighted for National Estimates |
|---|---|---|---|---|
| 2020 | AK, CA, CO, CT, DC, FL, GA, HI, IA, IL, IN, KS, KY, MD, ME, MI, MN, MO, NC, ND, NE, NJ, NV, NY, OH, OK, OR, PA, SC, SD, TN, TX, UT, VT, WI | 2,899 | 7,828,310 | 10,337,699 |
| 2019 | AK, CA, CO, CT, DC, FL, GA, HI, IA, IL, IN, KS, KY, MD, ME, MI, MN, MO, NC, ND, NE, NJ, NV, NY, OH, OK, OR, PA, SC, SD, TN, TX, UT, VT, WI | 2,958 | 8,994,101 | 11,880,487 |
| 2018 | CA, CO, CT, DC, FL, GA, IA, IL, IN, KS, KY, MD, ME, MI, MN, MO, NC, ND, NE, NJ, NV, NY, OH, OK, OR, PA, SC, SD, TN, TX, VT, WI (HI and UT data were not available) | 2,699 | 7,693,084 | 10,696,131 |
| 2017 | CA, CO, CT, DC, FL, GA, IA, IL, IN, KS, KY, MD, ME, MI, MN, MO, NC, ND, NE, NJ, NV, NY, OH, OK, OR, PA, SC, SD, TN, TX, UT, VT, WI (HI data were not available) | 2,737 | 7,647,636 | 10,570,649 |
| 2016 | CA, CO, CT, DC, FL, GA, HI IA, IL, IN, KS, KY, MD, ME, MI, MN, MO, NC, ND, NE, NJ, NV, NY, OH, OK, OR, PA, SC, SD, TN, TX, UT, VT, WI | 2,751 | 7,608,879 | 10,623,113 |
| Abbreviations: AS, Ambulatory Surgery; NASS, Nationwide Ambulatory Surgery Sample. | ||||
The 2020 NASS sample comprises data from 35 HCUP Partner organizations (34 States and the District of Columbia). Appendix A, Figure A.1 represents the geographic distribution of the HCUP Partner organizations that contributed to the 2020 NASS. The HCUP NASS States with the District of Columbia account for 82.7 percent of the U.S. population in 2020, an estimated 67 percent of hospital-owned facilities performing ambulatory surgeries, and an estimated 75.7 percent of ambulatory surgery encounters. Details on the percentage of population, encounters, and facilities by region are provided in Appendix A, Table A.4 and Appendix A, Table A.5.
The NASS is limited to encounters with at least one in-scope ambulatory surgery on the record, performed at hospital-owned facilities. In-scope ambulatory surgeries are defined based on the following factors:
Although encounters are limited to those with at least one in-scope ambulatory surgery on the record, the NASS Supplemental File provides information on other surgical and nonsurgical procedures performed during these encounters (see Section 1.3).
1.2 Data Restrictions
Some HCUP Partner organizations that contributed data to the NASS imposed restrictions on the release of certain data elements. In addition, because of confidentiality laws, some data sources were prohibited from providing HCUP with encounter records that indicated specific medical conditions, such as HIV/AIDS or behavioral health conditions. Detailed information on these restrictions is available in Appendix C.
1.3 File Structure of the NASS
The NASS is delivered as a set of related files. A hospital file lists hospitals in the NASS along with hospital attributes (e.g., teaching status, bed size category) as well as the encounter weight and post-stratification stratum information. An encounter file links to the hospital table and contains information on the selected ambulatory surgery encounter (e.g., patient age, expected source of payment, diagnoses), including information about in-scope ambulatory surgeries. A related supplemental file contains entries for out-of-scope procedures with a key linking to the encounter file. Finally, a diagnosis and procedure group file contains information about diagnosis groupings with a key linking to the encounter file. (Note that this file is not available in the 2016 or 2017 NASS.)
Hospital File: This hospital-level file contains one observation for each hospital included in the NASS, along with encounter weight and stratum data elements. For 2020, the NASS Hospital File has 2,899 hospital-specific records. A list of data elements in the Hospital File is provided in Appendix D, Table D.1.
Encounter File: This encounter-level file contains 100 percent of ambulatory surgery encounters containing an in-scope ambulatory surgery from hospital-owned facilities in participating States and the District of Columbia that meet facility inclusion criteria. For 2020, the NASS Encounter File has about 7.8 million ambulatory surgery encounter records (unweighted). Refer to Appendix D, Table D.2 for a list of data elements in the NASS Encounter File.
Supplemental File: This encounter-level file contains information on procedures that were performed during encounters recorded in the Encounter File but not considered to be in-scope ambulatory surgeries in the NASS. The Supplemental File contains about 5.8 million records for 2020. Procedures included on the Supplemental File are limited to CPT procedure codes. HCPCS Level II codes were excluded from the Supplemental File. Refer to Appendix D, Table D.3 for a list of data elements in the NASS Supplemental File.
Diagnosis and Procedure Groups File: Available beginning with the 2020 NASS, this encounter-level file contains information about International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis groups and comorbidity indicators for all diagnoses associated with encounters recorded in the Encounter File, derived from the Clinical Classifications Software Refined (CCSR) for ICD-10-CM Tool4 and Elixhauser Comorbidity Software Refined for ICD-10-CM.5 Refer to Appendix D, Table D.4 for a list of data elements in the NASS Diagnosis and Procedure Groups File.
1.4 NASS Data Elements
The coding of data elements in the NASS is consistent with the coding in other HCUP databases. The following three objectives guided the definition of data elements in all HCUP databases:
More information on the coding of HCUP data elements is available on the HCUP User Support (HCUP-US) website (www.hcup-us.ahrq.gov/db/coding.jsp).
After analyzing the availability of information from the HCUP Partner organizations, a set of common fields to be available in the NASS was created. The NASS contains more than 100 clinical and nonclinical variables, such as the following:
For comprehensive information about the NASS data elements, please refer to the NASS documentation on the HCUP-US website (www.hcup-us.ahrq.gov/db/nation/nass/nassdbdocumentation.jsp).
2 GETTING STARTED
The HCUP NASS is distributed as comma-separated value (CSV) files delivered via secure digital download from the Online HCUP Central Distributor. The files are compressed and encrypted with SecureZIP® from PKWARE®.
The NASS product is downloaded in a single zipped file, which contains several data-related files and accompanying documentation. The four data-related files include the following compressed files:
To load and analyze the NASS data on a computer, users will need the following:
The total size of the CSV version of the NASS is 11.8 GB. The NASS files loaded into SAS are about 5.7 GB. Most SAS data steps will require twice the storage space of the file so that the input and output files can coexist.
With a file of this size, space easily could become a problem in a multistep program. It is not unusual to have several versions of a file marking different steps while preparing it for analysis, and there may be more versions for the actual analyses. Therefore, users should plan carefully because the amount of space required could escalate rapidly.
2.1 Decompressing the NASS Files
To extract the data files from the compressed download file, follow these steps:
2.2 Downloading and Running the Load Programs
Programs to load the data into SAS, SPSS, or Stata are available on the HCUP-US website. To download and run the load programs, follow these steps:
NOTE: Prior to the 2020 NASS, the Encounter File and Supplemental File load programs use the same variable names for the array of CPT codes (e.g., CPT1) and their associated CCS-Services and Procedures categories (e.g., CCSCPT1). When merging the Encounter and Supplemental Files, this can result in CPT and CCS-Services and Procedures codes being overwritten unintentionally in one file or the other. Starting with the 2020 NASS, the Supplemental File load program uses the variable names SupCPTn and SupCPTCCSn, where n indicates the order in the CPT array.
2.3 NASS Documentation
Comprehensive documentation for the NASS files is available on the HCUP-US website (www.hcup-us.ahrq.gov/db/nation/nass/nassdbdocumentation.jsp). Users of the NASS can access complete file documentation, including variable notes, file layouts, summary statistics, and related technical reports. Similarly, data users can download SAS, SPSS, and Stata load programs. These important resources help the user understand the structure and content of the NASS and aid in using the database. Appendix A, Table A.2 details the comprehensive NASS documentation available on HCUP-US.
2.4 HCUP Online Tutorials
For additional assistance, the Agency for Healthcare Research and Quality (AHRQ) has created the HCUP Online Tutorial Series, a series of free, interactive courses that provide information on using HCUP data and tools and training on technical methods for conducting research with HCUP data. Topics include an HCUP Overview Course and these tutorials:
Other tutorials about the design or use of the HCUP databases are also available, and new tutorials are added periodically. The Online Tutorial Series is located on the HCUP-US website at www.hcup-us.ahrq.gov/tech_assist/tutorials.jsp.
3 METHODS
3.1 Creation of the NASS
Creation of the NASS requires the following steps:
The relationship between the NASS universe, the SASD sample, and the NASS sampling frame is portrayed in Figure 1. The predictive model for hospital ambulatory surgery encounter volume is developed using the NASS sampling frame hospitals and then is applied to all other hospitals not in the sampling frame to generate the encounter universe. In 2020, the NASS sample and sampling frame were identical because 100 percent of hospitals were sampled.
Figure 1. NASS Hospital Universe, SASD Sample, and NASS Sampling Frame
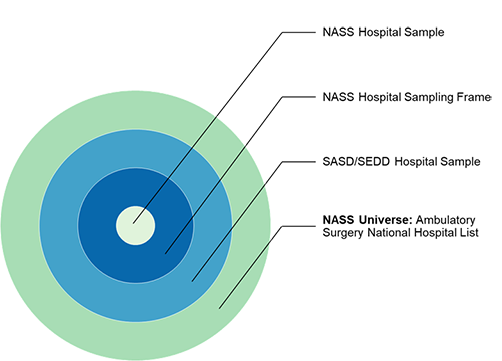
Abbreviations: NASS, Nationwide Ambulatory Surgery Sample; SASD, State Ambulatory Surgery and Services Databases.
Four concentric circles illustrating the relationship between the NASS universe, the SASD sample, and the NASS sampling frame. The innermost, smallest circle represents the NASS hospital sample. The next largest circle represents the NASS hospital sampling frame. The next largest circle represents the SASD hospital sample. The outermost, largest circle represents the NASS universe (i.e., the Ambulatory Surgery National Hospital List).
The following sections describe several of the NASS development steps in greater detail.
3.2 Selection of In-Scope Ambulatory Surgeries
3.2.1 Definition of In-Scope Ambulatory Surgery
HCUP Surgery Flag Software7 was used to identify surgical procedures of interest for the NASS. The Surgery Flag Software classifies CPT procedure codes as narrow, broad, or neither. The NASS focuses on surgeries in the narrow class, or in-scope ambulatory surgeries. These surgeries consist of procedures that (1) require the use of an operating room, (2) penetrate or break the skin, and (3) involve regional anesthesia, general anesthesia, or sedation to control pain. Examples of in-scope procedures include cataract surgery, cholecystectomy, appendectomy, gastric bypass, hysterectomy, hernia repair, spinal fusion, and hip replacement. The following three procedures, which are primarily performed for a diagnostic purpose, are assigned a narrow surgery flag based on the degree of their invasiveness: biopsies if the procedure is within an internal organ (e.g., brain, deep cervical node, stomach), thoracotomy with or without biopsy, and exploratory laparotomy with or without biopsy.
Starting with v2019.2 of the HCUP Surgery Flag Software (used for the 2018–2019 NASS), narrow surgeries are identified in the following ranges of CPT codes: surgical, emerging technology, radiology, and medical (excluding the evaluation and management codes). Prior to that radiology and medical CPTs were not included in the HCUP Surgery Flag Software. For the 2020 NASS, v2020.1 of the HCUP Surgery Flag Software (which includes the same types of procedures as v2019.2) was used because v2020.1 is relevant to CPT codes valid in calendar year 2020.
3.2.2 Selection of In-Scope Ambulatory Surgeries
Several selection criteria were used to define in-scope ambulatory surgeries for the NASS. Prior to application of selection criteria, all in-scope ambulatory surgeries identified by HCUP Surgery Flag Software (as narrow) were grouped in categories defined by CCS for Services and Procedures.8
Beginning with data year 2019, the following criteria were applied at the CCS-Services and Procedures category level:
The final set of included, or in-scope, CCS-Services and Procedures categories for the 2020 NASS is provided in Appendix B. Appendix B also includes a running list of changes to the in-scope procedure groups over time.
Prior to data year 2019, the following criteria were applied at the CCS-Services and Procedures category level:
Figure 2 illustrates the relationship between ambulatory surgeries, major ambulatory surgeries, and in-scope major ambulatory surgeries.
Note that although encounters are limited to those with at least one in-scope ambulatory surgery on the record, the NASS Supplemental File provides information on other (or out-of-scope) procedures performed during these encounters.
Figure 2. Ambulatory Surgeries, Major Ambulatory Surgeries, and In-Scope Ambulatory Surgeries
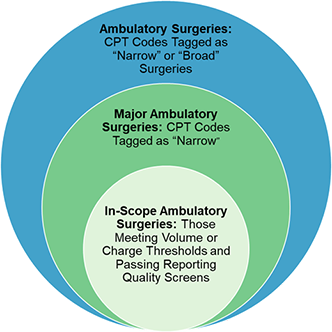
Abbreviation: CPT, Current Procedural Terminology.
Three overlapping circles illustrating the relationship between ambulatory surgeries, major ambulatory surgeries, and in-scope ambulatory surgeries. The smallest circle represents in-scope ambulatory surgeries (i.e., those meeting volume or charge thresholds and passing reporting quality screens). The next largest circle, which encapsulates the smallest circle, represents major ambulatory surgeries (i.e., CPT codes tagged as "narrow"). The largest circle, which encapsulates the smaller two circles, represents ambulatory surgeries (i.e., CPT codes tagged as "narrow" or "broad" surgeries).
3.3 Sampling Design of the NASS
The NASS is a stratified cluster sample of in-scope ambulatory surgery encounters (see Section 3.2) occurring in hospital-owned facilities. The main objective of a stratified sample is to ensure that it is representative of the target universe with respect to factors in the stratification scheme. In this section, we summarize the NASS setting and universe definition, the process for constructing the sampling frame, the sample strata, the sampling plan, and the calculation of sample weights.
3.3.1 Ambulatory Surgery Setting and Universe Definition
Ambulatory surgeries are performed in hospital-owned facilities, nonhospital-owned ambulatory surgery centers (ASCs), or office settings. In this context, office means a place of service that is neither a hospital-owned facility nor an ASC. The office setting may include professional facilities with procedure rooms or surgical suites.
HCUP Partners provide information on ambulatory surgeries in hospital-owned facilities. About half of the Partners also provide ambulatory surgery data from facilities that are not hospital owned. The designation of a facility as hospital owned is specific to its financial relationship with a hospital that provides inpatient care and is not related to its physical location. Hospital-owned ambulatory surgery and other outpatient care facilities may be contained within the hospital, physically attached to the hospital, or located in a different geographic area. The designation as hospital owned means that HCUP can verify that the hospital is billing for this service.
The NASS is restricted to in-scope ambulatory surgeries performed in the hospital-owned facilities, either in the hospital itself or in physically separate hospital-owned facilities. There are two reasons for this restriction. First, the SASD have more than twice as many hospital-owned facilities as facilities that are not hospital owned. Second, although the HCUP hospital sampling frame is well understood, much less is known about the HCUP sample of surgery facilities that are not hospital owned compared with all freestanding ASCs.
In addition to restricting attention to the hospital-owned facilities, facilities are limitied to U.S. community hospitals, defined as "all non-Federal, short-term, general, and other specialty hospitals, excluding hospital units of institutions."10 Noncommunity hospitals are excluded because of inconsistent capture of data across HCUP States. Additionally, community hospitals that are either rehabilitation or long-term acute care (LTAC) facilities are excluded because these hospitals treat a unique patient population that has longer stays and higher costs.
A key challenge for the NASS design is the creation of national in-scope ambulatory surgery encounter volume estimates (encounter universe), tabulated in strata used in the sampling design. National estimates do not exist for several reasons, but the most important is the definition of ambulatory surgery itself. Organizations collecting survey information from hospitals, such as the AHA, rely on verbal descriptions of ambulatory surgery.11 These descriptions leave room for interpretation and result in significant variation in which encounters hospitals report as ambulatory surgeries. In contrast, hospitals generally report total inpatient admissions, births, and emergency department visits with reasonable accuracy.
The NASS uses a CPT code- and data-based definition of in-scope ambulatory surgeries (see Section 3.2). Self-reported hospital ambulatory surgery volumes from the AHA may or may not be consistent with the HCUP definition of in-scope ambulatory surgeries, and it is challenging to ascertain that consistency. Consequently, rather than using an external reference source for in-scope ambulatory surgery volumes, the NASS universe of in-scope ambulatory surgery encounters was constructed by combining observed encounter volumes for hospitals in the NASS sampling frame and estimated encounter volumes for all other hospitals performing in-scope ambulatory surgeries. Estimated encounter volumes were generated using a predictive model, described in Section 3.4.1.
3.3.2 Generating the Ambulatory Surgery National Hospital List
A crucial step in developing the NASS was generating a list of hospitals performing in-scope ambulatory surgery outside the NASS sampling frame and hospital-specific predictor variables to compute estimated encounters using a predictive model (see Section 3.4.1).
Hospitals were included in the national list if they were a community hospital. Rehabilitation and LTAC hospitals were excluded. Hospitals reporting no outpatient surgeries in the AHA Annual Survey were then excluded from the national list.
Model predictor variables were obtained from the AHA Annual Survey (for HCUP SASD hospitals and hospitals reporting outpatient surgeries in the AHA Annual Survey). See Table 2 for a description of the predictor variables obtained from AHA.
3.4 NASS Sampling Frame
Selection of SASD hospitals for the NASS sampling frame was limited to facilities owned by community hospitals, excluding rehabilitation and LTAC hospitals.12
Additional restrictions imposed for the NASS sampling frame were that the hospital (1) have no gross irregularities in quarterly reporting volume, (2) submit data to the SASD in all four quarters of 2020, and (3) not have an unusually low volume of encounters containing an in-scope ambulatory surgery.
A comparison between the NASS hospital universe and the final NASS sample is provided in Appendix A, Table A.3.
3.4.1 NASS Encounter Predictive Model
Creation of the in-scope ambulatory surgery encounter universe requires a method for estimating the volume of encounters containing in-scope ambulatory surgeries for hospitals outside the NASS sampling frame. This estimation was accomplished by building a predictive model for encounters using data for the 2,899 hospitals in the NASS sampling frame.
The hospital-specific number of encounters containing at least one in-scope ambulatory surgery was the outcome variable in the model. A model predicting the number of in-scope ambulatory surgery encounters per hospital was developed using the NASS sampling frame hospitals. Predictor variables used in the model are reported in Table 2.
Table 2. Independent Variables Included in Encounter Predictive Model
| Category | Independent Variable |
|---|---|
| Ownership | Voluntary, not for profit |
| Proprietary, for profit | |
| Local or State governments | |
| Location and teaching status | Rural location |
| Urban nonteaching | |
| Urban teaching | |
| Census region | Midwest |
| Northeast | |
| South | |
| West | |
| Hospital size (number of beds) | 001-025 |
| 026-049 | |
| 050-099 | |
| 100-199 | |
| 200-299 | |
| 300-399 | |
| 400-499 | |
| 500+ | |
| AHA Annual Survey: self-reported outpatient surgery volume | Log scale |
| Abbreviation: AHA, American Hospital Association. | |
3.4.2 Post-Stratification for Weighting
Post-stratification for the purpose of weighting allows for compensation of any over- or under-represented types of hospitals in the sampling frame (the NASS) with respect to the distribution in the target universe. Hospital characteristics for post-stratification were selected using results from the encounter predictive model (which quantify the importance of stratification factors in encounter volume variation) and a study of the current NIS and NEDS stratification schemes. Table 3 contains values for the NASS stratification variables: census region, bed size category,13 location and teaching status, and ownership.14 There are 108 possible strata (i.e., unique combinations of region, bed size, location/teaching status, and ownership categories).
Table 3. NASS Stratification Variables
| Stratum | Code | Label |
|---|---|---|
| Census region | 1 | North |
| 2 | Midwest | |
| 3 | South | |
| 4 | West | |
| Bed size category | 1 | Small (depends on region, location, and teaching status) |
| 2 | Medium (depends on region, location, and teaching status) | |
| 3 | Large (depends on region, location, and teaching status) | |
| Location and teaching status | 1 | Rural |
| 2 | Urban nonteaching | |
| 3 | Urban teaching | |
| Ownership | 1 | Local and State government |
| 2 | Voluntary, not for profit | |
| 3 | Proprietary, for profit | |
| Abbreviation: NASS, Nationwide Ambulatory Surgery Sample. | ||
A goal was established to have at least 10 hospitals assigned to each stratum with as many strata as possible having a sampling fraction greater than 0.20. 15
Assignment of hospitals to the initial stratification scheme of 108 levels results in a number of strata with fewer than 10 sampling frame hospitals small sampling fractions. In those cases, ownership category was collapsed, first by combining local and State government with voluntary hospitals.16 If the goal still was not achieved, all the ownership types were combined.
We used judgment when manually collapsing the strata to ensure that no single stratum had a large percentage of total encounter or hospital volume. This led to relaxing the number of sampling frame hospitals or sampling fraction criteria for some strata. After manual adjustments, the NASS had 62 strata for 2020. In the end, all strata had at least 10 hospitals and sampling fractions greater than 0.20.
3.5 Encounter Weights
To obtain nationwide estimates, encounter weights were developed combining the NASS universe of hospitals and encounters with the NASS sample hospitals and encounters.
Computation of sample weights is straightforward. Given a universe of encounter volumes in stratum s, the sample weight is computed as the ratio of NASS universe to sample encounter volumes so that the sample volume is inflated to agree with the universe volume within the stratum.
3.5.1 Frame Sampling Rate
For the 2020 NASS, all hospitals in the sampling frame were selected for inclusion in the NASS, resulting in an approximate 67 percent sample of universe hospitals.
3.5.2 Encounter Weights
Encounter weights were calculated by stratum. Within stratum s for hospital i, the universe weight for each encounter in the NASS sample was calculated as follows:
Wis(universe) = [Ns(universe) ÷ Ns(sample)] * (4 ÷ Qi),
where Wis(universe) is the encounter weight, Ns(universe) represents the number of ambulatory surgery encounters in the universe within stratum s, Ns(sample) is the number of ambulatory surgery encounters from sample hospitals selected for the NASS, and Qi represents the number of quarters of ambulatory surgery encounters contributed by hospital i to the NASS (for the 2020 NASS, Qi = 4 for all hospitals). Thus, each encounter's weight is equal to the number of universe ambulatory surgery encounters it represents in stratum s during that year. Wis(universe) is named DISCWT in the NASS encounter table (see Appendix D, Table D.2).
The 2020 NASS sampling frame required that all hospitals qualifying for the frame submit data in all four quarters of 2020.
4 HOW TO USE THE NASS FOR DATA ANALYSIS
This section provides a synopsis of special considerations for using the NASS.
4.1 Calculating National Estimates
To produce national estimates, weights MUST be used.
The in-scope ambulatory surgery encounter weight (DISCWT) in the NASS Encounter Table should be used for producing nationwide, encounter-level statistics where the ambulatory surgery encounter is the unit of analysis.
Because the NASS is a stratified cluster sample, proper statistical techniques must be used to calculate standard errors and confidence intervals. For detailed instructions, refer to the HCUP Methods Series report #2003-02, Calculating Nationwide Inpatient Sample (NIS) Variances for Data Years 2011 and Earlier, on the HCUP-US website (www.hcup-us.ahrq.gov/). The HCUP NIS prior to 2012 used a stratified sampling design similar to the NASS, so techniques appropriate for the NIS prior to 2012 also are appropriate for the NASS.
4.2 Choosing Data Elements for Analysis
For all data elements to be used in the analysis, the analyst first should perform descriptive statistics and examine the range of values, including the number of missing cases. When anomalies (such as large numbers of missing cases) are detected, descriptive statistics can be computed by region for that variable to determine whether there are region-specific differences. Sometimes, computing descriptive statistics by hospital can be helpful in detecting hospital-specific data anomalies.
4.3 ICD-10-CM Diagnosis Codes and CPT Procedure Codes
Each unique analysis should consider limitations related to ICD-10-CM and CPT procedure codes.
4.4 Missing Values
Missing data values can compromise the quality of estimates. For example, if the outcome for ambulatory surgery encounters with missing values is different from the outcome for ambulatory surgery encounters with valid values, then sample estimates for that outcome will be biased and inaccurately represent the ambulatory surgery utilization patterns. Several techniques are available to help overcome this bias. One strategy is to use imputation to replace missing values with acceptable values. Another strategy is to use sample weight adjustments to compensate for missing values. Descriptions of such data preparation and adjustment are outside the scope of this report; however, it is recommended that researchers evaluate and adjust for missing data, if necessary.
Alternatively, if the cases with and without missing values are assumed to be similar with respect to their outcomes, no adjustment may be necessary for estimates of means and rates because the nonmissing cases would be representative of the missing cases. However, some adjustment still may be necessary for the estimates of totals. Sums of data elements (such as aggregate ambulatory surgery charges) containing missing values would be incomplete because cases with missing values would be omitted from the calculations. Estimates of the sum of charges should use the product of the number of cases times the average charge to account for records with missing information.
4.5 Variance Calculations
It may be important for researchers to calculate a measure of precision for some estimates based on the NASS sample data. Variance estimates must account for both the sampling design and the form of the statistic. The NASS sampling design consists of a stratified, single-stage cluster sample. A stratified random sample of hospitals (clusters) providing in-scope ambulatory surgeries was drawn, and then all encounters with in-scope ambulatory surgeries were included from each selected hospital. To accurately calculate variances from the NASS, appropriate statistical software and techniques must be used. For detailed instructions, refer to the HCUP Methods Series report #2003-02, Calculating Nationwide Inpatient Sample (NIS) Variances for Data Years 2011 and Earlier, on the HCUP-US website (www.hcup-us.ahrq.gov/). The HCUP NIS prior to 2012 used a stratified sample design similar to the NASS, so techniques appropriate for the NIS prior to 2012 also are appropriate for the NASS.
If hospitals inside the sampling frame are like hospitals outside the frame, the sample hospitals can be treated as if they were randomly selected from the entire universe of hospitals within each stratum. Standard formulas for a stratified, single-stage cluster sample without replacement could be used to calculate statistics and their variances in most applications.
A multitude of statistics can be estimated from the NASS data. Several computer programs that calculate statistics and their variances from sample survey data are listed in Section 4.6. Some of these programs use general methods of variance calculations (e.g., the jackknife and balanced half-sample replications) that account for the sampling design. However, it may be desirable to calculate variances using formulas specifically developed for certain statistics.
These variance calculations are based on finite-sample theory, which is an appropriate method for obtaining cross-sectional, nationwide estimates of outcomes. According to finite-sample theory, the intent of the estimation process is to obtain estimates that are precise representations of the nationwide population at a specific point in time. In the context of the NASS, any estimates that attempt to accurately describe characteristics and interrelationships among hospitals and ambulatory surgery encounters during a specific year should be governed by finite-sample theory. Examples include estimates of expenditure and utilization patterns.
Alternatively, in the study of hypothetical population outcomes not limited to a specific point in time, the concept of a superpopulation may be useful. Analysts may be less interested in specific characteristics of the finite population (and time period) from which the sample was drawn than they are in hypothetical characteristics of a conceptual superpopulation from which any particular finite population in a given year might have been drawn. According to this superpopulation model, the nationwide population in a given year is only a snapshot in time of the possible interrelationships among hospital, market, discharge, encounter, or visit characteristics. In a given year, all possible interactions between such characteristics may not have been observed, but analysts may wish to predict or simulate interrelationships that may occur in the future.
Under the finite-population model, the variances of estimates approach zero as the sampling fraction approaches one. This is the case because the population is defined at that point in time and because the estimate is for a characteristic as it existed when sampled. This is in contrast to the superpopulation model, which adopts a stochastic viewpoint rather than a deterministic viewpoint. That is, the nationwide population in a particular year is viewed as a random sample of some underlying superpopulation over time. Different methods are used for calculating variances under the two sample theories. The choice of an appropriate method for calculating variances for nationwide estimates depends on the type of measure and the intent of the estimation process.
4.6 Computer Software for Weighted and Variance Calculations
Computer programs are readily available to perform weighted variance calculations. Several statistical programming packages allow weighted analyses.17 For example, nearly all SAS procedures incorporate weights. In addition, several statistical analysis programs have been developed to specifically calculate statistics and their standard errors from survey data. Version 8 or later of SAS contains procedures (PROC SURVEYMEANS and PROC SURVEYREG) for calculating statistics on the basis of specific sampling designs. Stata and SUDAAN® are two other common statistical software packages that perform calculations for numerous statistics arising from the stratified, single-stage cluster sampling design. Examples of the use of SAS, SUDAAN, and Stata to calculate NIS variances are presented in the special report Calculating Nationwide Inpatient Sample (NIS) Variances for Data Years 2011 and Earlier, on the HCUP-US website (www.hcup-us.ahrq.gov/). For a helpful review of programs to calculate statistics from survey data, visit the following website: www.hcp.med.harvard.edu/statistics/survey-soft/. ![]()
The NASS includes a Hospital File with variables required by these programs to calculate finite-population statistics. The file includes synthetic hospital identifiers (Primary Sampling Units, or PSUs), stratification variables, and stratum-specific totals for the numbers of ambulatory surgery encounters and hospitals so that finite-population corrections can be applied to variance estimates.
In addition to these subroutines, standard errors can be estimated by validation and cross-validation techniques. Depending on the analysis problem, a large number of observations may be available, and it may be feasible to set aside a part of the data for validation purposes. Standard errors and confidence intervals then can be calculated from the validation data.
If the analytic file is too small to set aside a large validation sample, cross-validation techniques may be used. For example, tenfold cross-validation would split the data into 10 subsets of equal size. The estimation would take place in 10 iterations. In each iteration, the outcome of interest is predicted for one-tenth of the observations by an estimate based on a model that is fit to the other nine-tenths of the observations. Unbiased estimates of error variance then are obtained by comparing the actual values to the predicted values obtained in this manner.
4.7 Limitations of the NASS
The NASS contains about 7.8 million ambulatory surgery encounter records and many clinical and nonclinical data elements. Many research studies can be conducted with the data, but some limitations should be considered:
The NASS contains encounter-level records, not patient-level records. This means that individual patients who visit a hospital facility for ambulatory surgery multiple times in 1 year may be present in the NASS multiple times. No uniform patient identifier is available that would allow a patient-level analysis to identify individuals with more than one ambulatory surgery encounter or to track outcomes or additional follow-up care received after an encounter. In contrast, some HCUP State databases may be used for this type of analysis.
The database includes only HCPCS Level I or CPT codes. HCPCS Level II codes are excluded.
4.8 Considerations for Trending Over Time
When conducting longitudinal analyses, users should exercise caution and consider several aspects of the NASS design and changes to the design over time.
Refer to Appendix E for a summary of CCS procedure category totals in the 2016-2020 NASS and contributing reasons for large changes over time. For the subset of CCS categories affected by NASS design changes, trend analyses based on CCS category are not recommended.
5 USER FEEDBACK AND QUESTIONS
HCUP would like to hear from data users regarding any suggestions, comments, or issues in using the NASS. Please contact HCUP User Support at hcup@ahrq.gov or (866) 290-HCUP (4287).
Appendix A: NASS Introductory Information
Table A.1. HCUP Partner Organizations Participating in the 2020 NASS
| State | Data Organization |
|---|---|
| Alaska | Alaska Department of Health Alaska State Hospital and Healthcare Association |
| California | California Department of Health Care Access and Information |
| Colorado | Colorado Hospital Association |
| Connecticut | Connecticut Hospital Association |
| District of Columbia | District of Columbia Hospital Association |
| Florida | Florida Agency for Health Care Administration |
| Georgia | Georgia Hospital Association |
| Hawaii | Hawaii Laulima Data Alliance Hawaii University of Hawai'i at Hilo |
| Illinois | Illinois Department of Public Health |
| Indiana | Indiana Hospital Association |
| Iowa | Iowa Hospital Association |
| Kansas | Kansas Hospital Association |
| Kentucky | Kentucky Cabinet for Health and Family Services |
| Maine | Maine Health Data Organization |
| Maryland | Maryland Health Services Cost Review Commission |
| Michigan | Michigan Health & Hospital Association |
| Minnesota | Minnesota Hospital Association |
| Missouri | Missouri Hospital Industry Data Institute |
| Nebraska | Nebraska Hospital Association |
| Nevada | Nevada Department of Health and Human Services |
| New Jersey | New Jersey Department of Health |
| New York | New York State Department of Health |
| North Carolina | North Carolina Department of Health and Human Services |
| North Dakota | North Dakota (data provided by the Minnesota Hospital Association) |
| Ohio | Ohio Hospital Association |
| Oklahoma | Oklahoma State Department of Health |
| Oregon | Oregon Association of Hospitals and Health Systems Oregon Office of Health Analytics |
| Pennsylvania | Pennsylvania Health Care Cost Containment Council |
| South Carolina | South Carolina Revenue and Fiscal Affairs Office |
| South Dakota | South Dakota Association of Healthcare Organizations |
| Tennessee | Tennessee Hospital Association |
| Texas | Texas Department of State Health Services |
| Utah | Utah Department of Health |
| Vermont | Vermont Association of Hospitals and Health Systems |
| Wisconsin | Wisconsin Department of Health Services |
| Abbreviation: HCUP, Healthcare Cost and Utilization Project; NASS, Nationwide Ambulatory Surgery Sample. | |
Figure A.1. HCUP States and the District of Columbia Included in the 2020 NASS
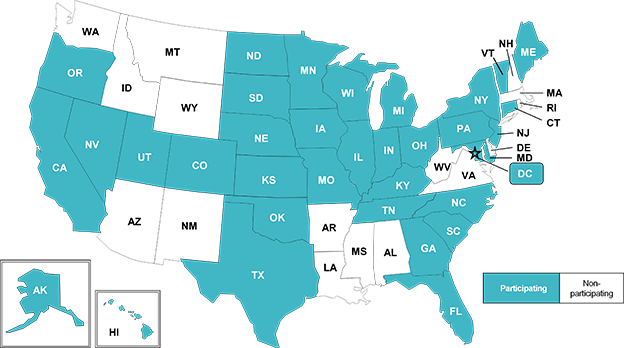
Abbreviation: HCUP, Healthcare Cost and Utilization Project; NASS, Nationwide Ambulatory Surgery Sample.
(A map of the United States showing which HCUP States are included in the 2020 NASS. Shaded States represent the 35 Partners that provide Ambulatory Surgery and Services data included in the NASS (Alaska, California, Colorado, Connecticut, District of Columbia, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kansas, Kentucky, Maine, Maryland, Michigan, Minnesota, Missouri, Nebraska, Nevada, New Jersey, New York, North Carolina, North Dakota, Ohio, Oklahoma, Oregon, Pennsylvania, South Carolina, South Dakota, Tennessee, Texas, Utah, Vermont, and Wisconsin.) Non participating states are Alabama, Arkansas, Arizona, Delaware, Idaho, Louisiana, Massachusetts, Mississippi, Montana, New Hampshire, New Mexico, Rhode Island, Virginia, West Virginia, Washington, Wyoming,.
Table A.2. NASS-Related Reports and Database Documentation Available on the HCUP-US Website
Description of the NASS Database
Restrictions on the Use
File Specifications and Load Programs
Data Elements
Additional Resources for NASS Data Elements
|
NASS
HCUP Tools: Labels and Formats
Obtaining HCUP Data |
|
| Abbreviation: CCSR, Clinical Classification Software Refined; HCUP, Healthcare Cost and Utilization Project; ICD-10-CM/PCS, International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System; NASS, Nationwide Ambulatory Surgery Sample; US, User Support. | ||
| Sample | Description | Number of Hospitals Providing Outpatient Surgery | Number of In-Scope Ambulatory Surgery Encounters |
|---|---|---|---|
| 2020 target universe | Community hospitals (excluding rehabilitation and LTAC) | 4,352a | 10,337,699b |
| 2020 NASS | Sample of target universe drawn from the sampling frame | 2,899 | 7,828,310 |
| Abbreviation: LTAC, long-term acute care; NASS, Nationwide Ambulatory Surgery Sample. a Estimated. See section 3.3.2. b Estimated. See section 3.4.1. | |||
| Census Region | 2020 Population States in NASS Sampling Frame | 2020 Population States Not in NASS Sampling Frame | Total 2020 Population | States in NASS Sampling Frame: Percent of Total Population |
|---|---|---|---|---|
| Midwest | 68,316,744 | 0 | 68,316,744 | 100 |
| Northeast | 46,532,895 | 9,316,974 | 55,849,869 | 83.3 |
| South | 99,736,437 | 26,926,317 | 126,662,754 | 78.7 |
| West | 57,943,606 | 20,711,150 | 78,654,756 | 73.7 |
| Total | 272,529,682 | 56,954,441 | 329,484,123 | 82.7 |
| Abbreviation: NASS, Nationwide Ambulatory Surgery Sample. Source: Annual Estimates of the Resident Population for the United States, Regions, States, the District of Columbia, and Puerto Rico: April 1, 2010 to July 1, 2019; April 1, 2020; and July 1, 2020 (NST-EST2020), Population Division, U.S. Census Bureau, www.census.gov/programs-surveys/popest/technical-documentation/research/evaluation-estimates/2020-evaluation-estimates/2010s-state-total.html. | ||||
| Census Region | Encounters | Facilities | ||||
|---|---|---|---|---|---|---|
| No. of Ambulatory Surgery Encounters (Unweighted) | No. of Ambulatory Surgery Encounters (Weighted)a | Unweighted Encounters: Weighted Encounters, % | No. of NASS Sample Hospitals | No. of Hospitals Performing Ambulatory Surgeryb | NASS Sample Hospitals: Hospitals Performing Ambulatory Surgery, % | |
| Midwest | 2,496,947 | 2,685,868 | 93.0 | 1,076 | 1,324 | 81.3 |
| Northeast | 1,359,342 | 1,690,562 | 80.4 | 406 | 541 | 75.0 |
| South | 2,654,907 | 3,900,417 | 68.1 | 936 | 1,601 | 58.5 |
| West | 1,317,114 | 2,060,852 | 63.9 | 481 | 886 | 54.3 |
| Total | 7,828,310 | 10,337,699 | 75.7 | 2,899 | 4,352 | 66.6 |
| Abbreviation: NASS, Nationwide Ambulatory Surgery Sample. a Estimated. See section 3.3.2. b Estimated. See section 3.4.1. | ||||||
Appendix B: 2020 NASS In-Scope Ambulatory Surgeries
Table B.1. NASS In-Scope Ambulatory Surgeries Identified by Clinical Classifications Software (CCS) for Services and Procedure Categories
| CCS for Services and Procedures Category | Description | Data Years in Scope for the NASS Sample |
|---|---|---|
| 003 | Laminectomy, excision intervertebral disc | 2016-2020 |
| 006 | Decompression peripheral nerve | 2016-2020 |
| 009 | Other OR therapeutic nervous system procedures | 2016-2020 |
| 010 | Thyroidectomy, partial or complete | 2016-2020 |
| 012 | Other therapeutic endocrine procedures | 2016-2020 |
| 013 | Corneal transplant | 2016-2020 |
| 014 | Glaucoma procedures | 2016-2020 |
| 015 | Lens and cataract procedures | 2016-2020 |
| 016 | Repair of retinal tear, detachment | 2016-2020 |
| 017 | Destruction of lesion of retina and choroid | 2019-2020 |
| 019 | Other therapeutic procedures on eyelids, conjunctiva, cornea | 2018-2020 |
| 020 | Other intraocular therapeutic procedures | 2018-2020 |
| 021 | Other extraocular muscle and orbit therapeutic procedures | 2016-2020 |
| 022 | Tympanoplasty | 2016-2020 |
| 023 | Myringotomy | 2016-2020 |
| 024 | Mastoidectomy | 2016-2020 |
| 026 | Other therapeutic ear procedures | 2016-2020 |
| 028 | Plastic procedures on nose | 2016-2020 |
| 030 | Tonsillectomy and/or adenoidectomy | 2016-2020 |
| 033 | Other OR therapeutic procedures on nose, mouth and pharynx | 2016-2020 |
| 042 | Other OR therapeutic procedures on respiratory system | 2016-2020 |
| 043 | Heart valve procedures | 2019-2020 |
| 045 | Percutaneous transluminal coronary angioplasty (PTCA)a | 2016, 2017, 2020 |
| 048 | Insertion, revision, replacement, removal of cardiac pacemaker or cardioverter/defibrillator | 2016-2020 |
| 049 | Other OR heart procedures | 2016-2020 |
| 053 | Varicose vein stripping, lower limb | 2016-2018 |
| 057 | Creation, revision and removal of arteriovenous fistula or vessel-to-vessel cannula for dialysis | 2016-2020 |
| 061 | Other OR procedures on vessels other than head and neck | 2016-2020 |
| 063 | Other non-OR therapeutic cardiovascular proceduresa | 2016, 2017 |
| 067 | Other therapeutic procedures, hemic and lymphatic system | 2016-2020 |
| 078 | Colorectal resection | 2016-2020 |
| 080 | Appendectomy | 2016-2020 |
| 081 | Hemorrhoid procedures | 2018-2020 |
| 084 | Cholecystectomy and common duct exploration | 2016-2020 |
| 085 | Inguinal and femoral hernia repair | 2016-2020 |
| 086 | Other hernia repair | 2016-2020 |
| 087 | Laparoscopy | 2016-2020 |
| 094 | Other OR upper GI therapeutic procedures | 2016-2020 |
| 095 | Other non-OR lower GI therapeutic proceduresa | 2016, 2017 |
| 096 | Other OR lower GI therapeutic procedures | 2016-2020 |
| 099 | Other OR gastrointestinal therapeutic procedures | 2016-2020 |
| 100 | Endoscopy and endoscopic biopsy of the urinary tract | 2016, 2017 |
| 101 | Transurethral excision, drainage, or removal urinary obstruction | 2018-2020 |
| 104 | Nephrectomy, partial or complete | 2018-2020 |
| 106 | Genitourinary incontinence procedures | 2016-2020 |
| 109 | Procedures on the urethra | 2016-2020 |
| 112 | Other OR therapeutic procedures of urinary tract | 2016-2020 |
| 113 | Transurethral resection of prostate (TURP) | 2016-2020 |
| 114 | Open prostatectomy | 2016-2020 |
| 117 | Other non-OR therapeutic procedures, male genitala | 2016, 2017 |
| 118 | Other OR therapeutic procedures, male genital | 2016-2020 |
| 119 | Oophorectomy, unilateral and bilateral | 2016-2020 |
| 120 | Other operations on ovary | 2016, 2020 |
| 121 | Ligation of fallopian tubes | 2016-2020 |
| 122 | Removal of ectopic pregnancy | 2016-2020 |
| 124 | Hysterectomy, abdominal and vaginal | 2016-2020 |
| 125 | Other excision of cervix and uterus | 2016-2020 |
| 129 | Repair of cystocele and rectocele, obliteration of vaginal vault | 2016-2020 |
| 130 | Other diagnostic procedures, female organs | 2018 |
| 132 | Other OR therapeutic procedures, female organs | 2016-2020 |
| 141 | Other therapeutic obstetrical procedures | 2016, 2017 |
| 142 | Partial excision bone | 2016-2020 |
| 143 | Bunionectomy or repair of toe deformities | 2016-2020 |
| 144 | Treatment, facial fracture or dislocation | 2016-2020 |
| 145 | Treatment, fracture or dislocation of radius and ulna | 2016-2020 |
| 146 | Treatment, fracture or dislocation of hip and femur | 2017, 2019, 2020 |
| 147 | Treatment, fracture or dislocation of lower extremity (other than hip or femur) | 2016-2020 |
| 148 | Other fracture and dislocation procedure | 2016-2020 |
| 149 | Arthroscopy | 2016-2020 |
| 150 | Division of joint capsule, ligament or cartilage | 2016-2020 |
| 151 | Excision of semilunar cartilage of knee | 2016-2020 |
| 152 | Arthroplasty knee | 2016-2020 |
| 153 | Hip replacement, total and partial | 2016-2020 |
| 154 | Arthroplasty other than hip or knee | 2016-2020 |
| 157 | Amputation of lower extremity | 2016-2020 |
| 158 | Spinal fusion | 2016-2020 |
| 160 | Other therapeutic procedures on muscles and tendons | 2016-2020 |
| 161 | Other OR therapeutic procedures on bone | 2016-2020 |
| 162 | Other OR therapeutic procedures on joints | 2016-2020 |
| 164 | Other OR therapeutic procedures on musculoskeletal system | 2016-2020 |
| 166 | Lumpectomy, quadrantectomy of breast | 2016-2020 |
| 167 | Mastectomy | 2016-2020 |
| 169 | Debridement of wound, infection or burn | 2020 |
| 170 | Excision of skin lesion | 2019-2020 |
| 171 | Suture of skin and subcutaneous tissue | 2016-2017, 2019-2020 |
| 172 | Skin graft | 2020 |
| 174 | Other non-OR therapeutic procedures on skin and breasta | 2016, 2017 |
| 175 | Other OR therapeutic procedures on skin and breast | 2016-2020 |
| 225 | Conversion of cardiac rhythm | 2016-2020 |
| 244 | Gastric bypass and volume reduction | 2016-2020 |
| Abbreviations: GI, gastrointestinal; NASS, Nationwide Ambulatory Surgery Sample; OR, operating room. a CCS categories 63, 95, 117, and 174 did not meet the criteria for inclusion beginning with the 2018 NASS because all in-scope surgeries were moved from these "non-OR therapeutic procedure" categories in an update to the CCS Services and Procedures Tool. For example, all in-scope surgeries in CCS 95, Other non-OR lower GI therapeutic procedures were reassigned to CCS 96, Other OR lower GI therapeutic procedures. Therefore, these in-scope surgeries are still included in the NASS, but with a different CCS category assignment than in previous NASS data years. CCS 45, PTCA, was removed from the NASS beginning with data year 2018 based on evidence of underreporting by NASS sample hospitals. Notes: Updates to the HCUP Surgery Flag Software for Services and Procedures changed the designation of several surgeries from major ("narrow") to not major ("broad" or "neither"), and vice versa. This affected the in-scope surgery volume and hospital-owned facility outpatient market share for multiple CCS categories, resulting in additions to and deletions from the NASS in-scope CCS procedure groups between data year 2017 and 2018. See www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp for more information on CCS Services and Procedures. |
||
Appendix C: Data Restrictions
Table C.1 enumerates the types of restrictions applied to the 2020 Nationwide Ambulatory Surgery Sample. Restrictions include the following types:
Table C.1. Data Restrictions
| Confidentiality of Hospitals Limitations on sampling to ensure hospital confidentiality:
|
|
| Confidentiality of Records Limitations on selected data elements to ensure patient confidentiality:
|
|
Limited Reporting of Diagnosis Codes for Medical Misadventures and Adverse Effects
|
|
Missing Information for Specific Populations of Patients
|
|
| Abbreviations: HCUP, Healthcare Cost and Utilization Project; NASS, Nationwide Ambulatory Surgery Sample. | |
| Type of Data Element | HCUP Data Element | Coding Notes |
|---|---|---|
| Encounter counts | TOTAL_AS_ENCOUNTERS | SASD encounters with at least one narrow surgery for this hospitala |
| N_DISC_U | Number of ambulatory surgery encounters for all hospitals in the stratum | |
| S_DISC_U | Number of ambulatory surgery encounters for sampled hospitals in the stratum | |
| Encounter weight | DISCWT | Encounter weight used to calculate national estimates |
| Encounter year | YEAR | Encounter year |
| Hospital characteristics | HOSP_BEDSIZE_CAT | Hospital bed size category: (1) 00-99, (2) 100-299, (3) 300+ |
| HOSP_LOCATION | Location of hospital: (0) rural, (1) urban | |
| HOSP_LOCTEACH | Location/teaching status of hospital: (1) rural, (2) urban nonteaching, (3) urban teaching | |
| HOSP_REGION | Region of hospital: (1) Northeast, (2) Midwest, (3) South, (4) West | |
| HOSP_TEACH | Teaching status of hospital: (0) nonteaching, (1) teaching | |
| NASS_STRATUM | Stratum used to sample hospital-owned facilities, includes geographic region, bed size category, location/teaching status, and control/ownership | |
| Hospital counts | N_HOSP_U | Number of hospitals in the stratum |
| S_HOSP_U | Number of sampled hospitals in the stratum | |
| NASS hospital identifier, synthetic | HOSP_NASS | Unique HCUP NASS hospital number, links to other NASS files, but not to other HCUP databases |
| Abbreviations: HCUP, Healthcare Cost and Utilization Project; NASS, Nationwide Ambulatory Surgery Sample. a Surgeries flagged as "narrow" in the HCUP Surgery Flag Software are defined as invasive therapeutic surgical procedures that typically require the use of an operating room and regional anesthesia, general anesthesia, or sedation. | ||
| Type of Data Element | HCUP Data Element | Coding Notes |
|---|---|---|
| Admission timing | AMONTH | Admission month coded from (1) January to (12) December |
| AWEEKEND | Admission on weekend: (0) admission on Monday-Friday, (1) admission on Saturday-Sunday | |
| Age at admission | AGE | Age in years coded 0-90 years. Any ages greater than 90 years were set to 90. |
| CPT procedure information | CPT1-CPT30 | In-scope CPT procedures on the record (maximum of 30) |
| CPTCCS1-CPTCCS30 | Clinical Classifications Software (CCS) category for in-scope CPT procedures | |
| NCPT_INSCOPE | Number of in-scope CPT procedures for this encounter | |
| Diagnosis information | I10_DX1-I10DX15 | ICD-10-CM diagnoses (maximum of 20) |
| I10_NDX | Number of diagnoses for this encounter | |
| I10_INJURY | Injury ICD-10-CM diagnosis reported on record | |
| I10_MULTINJURY | Multiple ICD-10-CM injuries reported on record | |
| Disposition of the patient | DISPUNIFORM | Disposition of patient, uniform coding: (1) routine; (2) transfer to short-term hospital; (5) other transfers, including skilled nursing facility, intermediate care, and another type of facility; (6) home healthcare; (7) against medical advice; (20) died in hospital; (99) discharged alive, destination unknown |
| Encounter timing | DQTR | Encounter quarter |
| YEAR | Encounter year | |
| Encounter weight | DISCWT | Encounter weight used to calculate national estimates |
| Hospital characteristics | NASS_STRATUM | Stratum used to sample hospital-owned facilities, includes geographic region, bed size category, location/teaching status, and control/ownership |
| Identifiers, synthetic | HOSP_NASS | Unique HCUP NASS hospital number, links to other NASS files but not to other HCUP databases |
| KEY_NASS | Unique HCUP NASS record number, links to NASS Supplemental and Diagnosis and Procedure Groups Files, but not to other HCUP databases | |
| National quartile for median household income of patient's ZIP Code | ZIPINC_QRTL | Median household income quartiles for patient's ZIP Code. For 2018, the median income quartiles are defined as (1) $1-$42,999, (2) $43,000-$53,999, (3) $54,000-$70,999, and (4) $71,000 or more. |
| Payer information | PAY1 | Expected primary payer, uniform: (1) Medicare, (2) Medicaid, (3) private including HMO, (4) self-pay, (5) no charge, (6) other |
| Race and ethnicity of patient | RACE | Race and ethnicity, uniform: (1) White, (2) Black, (3) Hispanic, (4) Asian or Pacific Islander, (5) Native American, (6) other |
| Sex of patient | FEMALE | Indicator of sex: (0) male, (1) female |
| Total charges | TOTCHG | Total charges for AS services, edited |
| Urban-rural location of patient's residence | PL_NCHS | Urban-rural designation for patient's county of residence: (1) large central metropolitan, (2) large fringe metropolitan, (3) medium metropolitan, (4) small metropolitan, (5) micropolitan, (6) not metropolitan or micropolitan |
| Abbreviations: AS, ambulatory surgery; CPT, Current Procedural Terminology; HCUP, Healthcare Cost and Utilization Project; HMO, health maintenance organization; ICD-10-CM, International Classification of Diseases, Tenth Revision, Clinical Modification; NASS, Nationwide Ambulatory Surgery Sample. | ||
| Type of Data Element | HCUP Data Element | Coding Notes |
|---|---|---|
| CPT procedure informationa | SupCPT1-SupCPT30 | Out-of-scope CPT procedures on the record (maximum of 30) |
| SupCPTCCS1-SupCPTCCS30 | Clinical Classifications Software (CCS) category for out-of-scope CPT procedures | |
| NCPT_NOTINSCOPE | Number of out-of-scope CPT procedures for this encounter | |
| Encounter year | YEAR | Encounter year |
| Identifiers, synthetic | HOSP_NASS | Unique HCUP NASS hospital number, links to other NASS files but not to other HCUP databases |
| KEY_NASS | Unique HCUP NASS record number, links to NASS Encounter and Diagnosis and Procedure Groups Files but not to other HCUP databases | |
| Abbreviations: CPT, Current Procedural Terminology; HCUP, Healthcare Cost and Utilization Project; NASS, Nationwide Ambulatory Surgery Sample. a Although some encounter records may have included Level II Healthcare Common Procedure Coding System (HCPCS) codes, this procedure information is limited to Level I HCPCS codes (i.e., CPT codes). | ||
| Type of Data Element | HCUP Data Element | Coding Notes |
|---|---|---|
| CCSR for ICD-10-CM diagnoses | DXCCSR_AAAnnn1 | Indication that at least one ICD-10-CM diagnosis on the record is included in CCSR AAAnnn |
| DXCCSR_DEFAULT_DX1 | Default CCSR for first-listed ICD-10-CM diagnosis | |
| DXCCSR_VERSION | Version of CCSR for ICD-10-CM diagnoses | |
| Elixhauser Comorbidity Software Refined for ICD-10-CM | CMR_aaa2 | Comorbidity measures (aaa) identified by the AHRQ Elixhauser Comorbidity Software Refined for ICD-10-CM diagnosis codes |
| CMR_VERSION | Version of the Elixhauser Comorbidity Measure Refined for ICD-10-CM | |
| Identifiers, synthetic | HOSP_NASS | Unique HCUP NASS hospital number, links to other NASS files but not to other HCUP databases |
| KEY_NASS | Unique HCUP NASS record number, links to NASS Encounter and Supplemental Files but not to other HCUP databases | |
| Abbreviations: CCSR, Clinical Classifications Software Refined; CPT, Current Procedural Terminology; HCUP, Healthcare Cost and Utilization Project; ICD-10-CM, International Classification of Diseases, Tenth Revision, Clinical Modification; NASS, Nationwide Ambulatory Surgery Sample. 1 Where aaa denotes the body system and nnn denotes the CCSR number within the body system. 2 Where aaa denotes the specific comorbidity measure. | ||
Appendix E: Encounter Totals by In-Scope Ambulatory Surgeries Identified by Clinical Classifications Software (CCS) for Services and Procedure Category, 2017–2020
Table E.1. Encounter Totals by In-Scope Ambulatory Surgeries Defined by Clinical Classifications Software (CCS) for Services and Procedure Category, 2017-2020
| CCS Category | Description | Total Encounters, N | Percentage Change, % | Potential Contributing Reasons for Change Over Time | |||||
|---|---|---|---|---|---|---|---|---|---|
| 2017 | 2018 | 2019 | 2020 | 2017-2018 | 2018-2019 | 2019-2020 | |||
| 003 | Laminectomy, excision intervertebral disc | 236,796 | 235,412 | 276,727 | 220,940.17 | -0.6 | 17.6 | -20.2 | |
| 006 | Decompression peripheral nerve | 353,638 | 351,346 | 387,555 | 332,053.71 | -0.6 | 10.3 | -14.3 | |
| 009 | Other OR therapeutic nervous system procedures | 102,208 | 95,330 | 115,510 | 99,886.48 | -6.7 | 21.2 | -13.5 | Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
| 010 | Thyroidectomy, partial or complete | 105,810 | 101,233 | 104,081 | 88,587.67 | -4.3 | 2.8 | -14.9 | |
| 012 | Other therapeutic endocrine procedures | 51,495 | 53,825 | 59,067 | 48,428.86 | 4.5 | 9.7 | -18.0 | |
| 013 | Corneal transplant | 18,961 | 19,091 | 20,318 | 15,904.23 | 0.7 | 6.4 | -21.7 | |
| 014 | Glaucoma procedures | 51,990 | 63,511 | 52,373 | 22.2 | -17.5 | Surgery Flag Software update: added as in scope for 2018; satisfied hospital outpatient market share threshold after reclassification of 2 CPT codes Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
||
| 015 | Lens and cataract procedures | 1,239,408 | 1,149,894 | 1,172,830 | 879,523 | -7.2 | 2.0 | -25 | |
| 016 | Repair of retinal tear, detachment | 96,040 | 96,345 | 99,232 | 85,378 | 0.3 | 3.0 | -14.0 | |
| 017 | Destruction of lesion of retina and choroid | 5,365 | 4,300 | -19.8 | Change to in-scope procedure criteria: in scope in 2019 because market share criterion was removed | ||||
| 019 | Other therapeutic procedures on eyelids, conjunctiva, cornea | 133,758 | 152,854 | 113,054 | 14.3 | -26.0 | Surgery Flag Software update: added as in scope for 2018; satisfied hospital outpatient market share threshold after reclassification of several CPT codes | ||
| 020 | Other intraocular therapeutic procedures | 85,208 | 88,491 | 71,129 | 3.9 | -19.6 | Surgery Flag Software update: added as in scope for 2018; satisfied hospital outpatient market share threshold after reclassification of 3 CPT codes | ||
| 021 | Other extraocular muscle and orbit therapeutic procedures | 62,476 | 56,429 | 60,624 | 48,741 | -9.7 | 7.4 | -19.6 | |
| 022 | Tympanoplasty | 29,354 | 48,328 | 52,013 | 44,158 | 64.6 | 7.6 | -15.1 | Surgery Flag Software update: volume increase in 2018 after 2 CPT codes were reclassified from broad to narrow |
| 023 | Myringotomy | 324,996 | 308,451 | 335,397 | 181,367 | -5.1 | 8.7 | -45.9 | |
| 024 | Mastoidectomy | 17,510 | 17,505 | 17,616 | 15,331 | 0.0 | 0.6 | -13.0 | |
| 026 | Other therapeutic ear procedures | 29,497 | 31,174 | 32,892 | 27,796 | 5.7 | 5.5 | -15.5 | |
| 028 | Plastic procedures on nose | 164,723 | 155,805 | 167,263 | 133,742 | -5.4 | 7.4 | -20.0 | |
| 030 | Tonsillectomy and/or adenoidectomy | 436,314 | 395,401 | 422,137 | 266,989 | -9.4 | 6.8 | -36.8 | |
| 033 | Other OR therapeutic procedures on nose, mouth and pharynx | 218,489 | 268,994 | 292,706 | 226,081 | 23.1 | 8.8 | -22.8 | Surgery Flag Software and CCS for Services and Procedures updates: overall volume increase in 2018 after reclassification of several CPT codes and reassignment of 1 narrow CPT code to CCS 33 from CCS 32 |
| 042 | Other OR therapeutic procedures on respiratory system | 36,275 | 34,996 | 35,164 | 30,176 | -3.5 | 0.5 | -14.2 | |
| 043 | Heart valve procedures | 4,609 | 3,961 | -14.1 | Change to in-scope procedure criteria: in scope in 2019 because this procedure exceeded the minimum threshold for total charges | ||||
| 045 | Percutaneous transluminal coronary angioplasty (PTCA) | 97,567 | Evidence of underreporting in 2016 and 2017 SASD: removed from in scope list for 2018 | ||||||
| 048 | Insertion, revision, replacement, removal of cardiac pacemaker or cardioverter/defibrillator | 276,914 | 260,471 | 265,870 | 257,606 | -5.9 | 2.1 | -3.1 | |
| 049 | Other OR heart procedures | 9,997 | 13,449 | 16,297 | 14,210 | 34.5 | 21.2 | -12.8 | Surgery Flag Software and CCS for Services and Procedures updates: overall volume increase in 2018 after 4 CPT codes were reclassified from narrow to broad and 1 narrow CPT code was reassigned to CCS 49 from CCS 63 Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe Addition of emergent surgeries: increase in 2019 after SEDD encounters were added to the NASS |
| 053 | Varicose vein stripping, lower limb | 29,557 | 7,865 | -73.4 | Surgery Flag Software update: volume decrease in 2018 after 2 CPT codes were reclassified from narrow to broad Change to in-scope procedure criteria: no longer in scope in 2019 because procedure did not meet minimum volume or charge threshold |
||||
| 057 | Creation, revision and removal of arteriovenous fistula or vessel-to-vessel cannula for dialysis | 155,498 | 158,579 | 156,776 | 141,773 | 2.0 | -1.1 | -9.6 | |
| 061 | Other OR procedures on vessels other than head and neck | 191,088 | 230,710 | 233,450 | 200,379 | 20.7 | 1.2 | -14.2 | |
| 063 | Other non-OR therapeutic cardiovascular procedures | 28,156 | CCS for Services and Procedures update: not in scope for 2018 after all narrow procedures were reassigned from CCS 63 to other CCS categories | ||||||
| 067 | Other therapeutic procedures, hemic and lymphatic system | 211,123 | 239,130 | 282,313 | 277,619 | 13.3 | 18.1 | -1.7 | |
| 078 | Colorectal resection | 12,590 | 13,077 | 13,810 | 11,608 | 3.9 | 5.6 | -15.9 | |
| 080 | Appendectomy | 174,534 | 170,952 | 278,430 | 263,929 | -2.1 | 62.9 | -5.2 | Addition of emergent surgeries: increase in 2019 after SEDD encounters were added to the NASS |
| 081 | Hemorrhoid procedures | 51,396 | 53,967 | 47,709 | 5.0 | -11.6 | Surgery Flag Software update: added as in scope for 2018; satisfied volume threshold after 6 CPT codes were reclassified to narrow | ||
| 084 | Cholecystectomy and common duct exploration | 585,438 | 559,911 | 606,943 | 541,909 | -4.4 | 8.4 | -10.7 | |
| 085 | Inguinal and femoral hernia repair | 458,721 | 446,464 | 456,556 | 399,740 | -2.7 | 2.3 | -12.4 | |
| 086 | Other hernia repair | 432,115 | 424,602 | 434,222 | 366,704 | -1.7 | 2.3 | -15.5 | |
| 087 | Laparoscopy | 72,596 | 76,976 | 81,420 | 77,524 | 6.0 | 5.8 | -4.8 | |
| 094 | Other OR upper GI therapeutic procedures | 12,619 | 21,563 | 26,266 | 21,694 | 70.9 | 21.8 | -17.4 | Surgery Flag Software and CCS for Services and Procedures updates: volume increase in 2018 after 1 CPT code was reclassified from broad to narrow and 1 narrow CPT code was reassigned to CCS 94 from CCS 95 Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
| 095 | Other non-OR lower GI therapeutic procedures | 5,405 | CCS for Services and Procedures update: not in scope for 2018 after all narrow procedures were reassigned from CCS 95 to CCS 96 | ||||||
| 096 | Other OR lower GI therapeutic procedures | 56,694 | 67,864 | 70,387 | 63,145 | 19.7 | 3.7 | -10.3 | |
| 099 | Other OR gastrointestinal therapeutic procedures | 32,470 | 18,708 | 18,679 | 17,034 | -42.4 | -0.2 | -8.8 | Surgery Flag Software update: volume decrease in 2018 after reclassification of 2 CPT codes were reclassified from narrow to broad |
| 100 | Endoscopy and endoscopic biopsy of the urinary tract | 17,309 | CCS for Services and Procedures update: not in scope for 2018 after all narrow procedures were moved from CCS 100 | ||||||
| 101 | Transurethral excision, drainage, or removal urinary obstruction | 151,887 | 158,548 | 149,311 | 4.4 | -5.8 | Surgery Flag Software update: added as in scope for 2018; satisfied volume threshold after reclassification of 8 CPT codes | ||
| 104 | Nephrectomy, partial or complete | 6,841 | 8,895 | 10,229 | 30.0 | 15.0 | Volume increase: added as in scope for 2018; satisfied volume threshold Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
||
| 106 | Genitourinary incontinence procedures | 109,746 | 112,970 | 115,272 | 93,999 | 2.9 | 2.0 | -18.5 | |
| 109 | Procedures on the urethra | 24,127 | 18,228 | 18,925 | 16,256 | -24.4 | 3.8 | -14.1 | Surgery Flag Software update: volume decrease in 2018 after 5 CPT codes were reclassified from narrow to neither |
| 112 | Other OR therapeutic procedures of urinary tract | 31,313 | 20,757 | 24,315 | 19,968 | -33.7 | 17.1 | -17.9 | Surgery Flag Software update and CCS for Services and Procedures update: volume decrease in 2018 after reclassification of 5 CPT codes and the reassignment of 1 narrow CPT code to CCS 112 from CCS 111 |
| 113 | Transurethral resection of prostate (TURP) | 81,782 | 84,765 | 89,707 | 79,868 | 3.6 | 5.8 | -11.0 | |
| 114 | Open prostatectomy | 7,914 | 28,017 | 38,372 | 40,903 | 254.0 | 37.0 | 6.6 | Reimbursement change: increased volume in 2018 after CMS removed laparoscopic prostatectomy from the inpatient-only lista Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
| 117 | Other non-OR therapeutic procedures, male genital | 8,412 | -100.0 | CCS for Services and Procedures update: not in scope for 2018 after all narrow procedures were reassigned from CCS 117 to CCS 118 | |||||
| 118 | Other OR therapeutic procedures, male genital | 208,931 | 170,126 | 177,839 | 162,850 | -18.6 | 4.5 | -8.4 | |
| 119 | Oophorectomy, unilateral and bilateral | 156,208 | 167,501 | 184,111 | 163,259 | 7.2 | 9.9 | -11.3 | |
| 120 | Other operations on ovary | 15,109 | 14,865 | 13,486 | -100.0 | -9.3 | Not in scope for 2018; did not satisfy outpatient hospital market share threshold Change to in-scope procedure criteria: in scope in 2019 because market share criterion was removed |
||
| 121 | Ligation of fallopian tubes | 89,543 | 76,698 | 65,993 | 45,659 | -14.3 | -14.0 | -30.8 | |
| 122 | Removal of ectopic pregnancy | 19,621 | 18,687 | 28,143 | 28,001 | -4.8 | 50.6 | -0.5 | Addition of emergent surgeries: increase in 2019 after SEDD encounters were added to the NASS |
| 124 | Hysterectomy, abdominal and vaginal | 372,422 | 382,869 | 399,826 | 362,270 | 2.8 | 4.4 | -9.4 | |
| 125 | Other excision of cervix and uterus | 19,695 | 51,258 | 51,878 | 45,368 | 160.3 | 1.2 | -12.5 | Surgery Flag Software update: volume increase in 2018 after 1 CPT code was reclassified from broad to narrow |
| 129 | Repair of cystocele and rectocele, obliteration of vaginal vault | 97,167 | 99,669 | 101,688 | 85,242 | 2.6 | 2.0 | -16.2 | |
| 130 | Other diagnostic procedures, female organs | 5,436 | -100.0 | Surgery Flag Software update: added as in scope for 2018; satisfied volume threshold after 2 CPT codes were reclassified from neither to narrow Change to in-scope procedure criteria: no longer in scope in 2019 because procedure did not meet minimum volume or charge threshold |
|||||
| 132 | Other OR therapeutic procedures, female organs | 227,217 | 226,192 | 236,321 | 204,583 | -0.5 | 4.5 | -13.4 | |
| 141 | Other therapeutic obstetrical procedures | 17,887 | Surgery Flag Software update: not in scope for 2018; did not satisfy volume threshold after reclassification of 2 CPT codes | ||||||
| 142 | Partial excision bone | 266,434 | 249,908 | 277,326 | 233,487 | -6.2 | 11.0 | -15.8 | |
| 143 | Bunionectomy or repair of toe deformities | 181,576 | 173,820 | 179,157 | 145,009 | -4.3 | 3.1 | -19.1 | |
| 144 | Treatment, facial fracture or dislocation | 48,670 | 43,661 | 43,810 | 34,101 | -10.3 | 0.3 | -22.2 | |
| 145 | Treatment, fracture or dislocation of radius and ulna | 115,873 | 117,738 | 135,863 | 132,590 | 1.6 | 15.4 | -2.4 | |
| 146 | Treatment, fracture or dislocation of hip and femur | 5,391 | 5,835 | 7,355 | 7,812 | 8.2 | 26.0 | 6.2 | Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe Addition of emergent surgeries: increase in 2019 after SEDD encounters were added to the NASS |
| 147 | Treatment, fracture or dislocation of lower extremity (other than hip or femur) | 160,680 | 165,542 | 193,280 | 190,041 | 3.0 | 16.8 | -1.7 | |
| 148 | Other fracture and dislocation procedure | 110,565 | 106,409 | 126,658 | 123,403 | -3.8 | 19.0 | -2.6 | |
| 149 | Arthroscopy | 94,560 | 88,407 | 99,699 | 75,626 | -6.5 | 12.8 | -24.1 | |
| 150 | Division of joint capsule, ligament or cartilage | 55,031 | 51,386 | 54,569 | 47,137 | -6.6 | 6.2 | -13.6 | |
| 151 | Excision of semilunar cartilage of knee | 417,884 | 383,794 | 404,838 | 327,348 | -8.2 | 5.5 | -19.1 | |
| 152 | Arthroplasty knee | 49,456 | 192,752 | 301,910 | 397,276 | 289.7 | 56.6 | 31.6 | Reimbursement change: increased volume in 2018 after CMS removed total knee arthroplasty from the inpatient-only lista Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
| 153 | Hip replacement, total and partial | 30,308 | 36,846 | 49,826 | 207,857 | 21.6 | 35.2 | 317.2 | Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe Increase in 2020 probably due to Medicare allowing total hip replacements to be performed in an ambulatory surgery settting. |
| 154 | Arthroplasty other than hip or knee | 55,611 | 57,934 | 66,148 | 62,708 | 4.2 | 14.2 | -5.2 | |
| 157 | Amputation of lower extremity | 40,221 | 42,802 | 48,970 | 43,724 | 6.4 | 14.4 | -10.7 | |
| 158 | Spinal fusion | 75,851 | 82,506 | 93,850 | 96,087 | 8.8 | 13.7 | 2.4 | |
| 160 | Other therapeutic procedures on muscles and tendons | 808,426 | 806,409 | 911,712 | 782,577 | -0.2 | 13.1 | -14.2 | |
| 161 | Other OR therapeutic procedures on bone | 281,555 | 259,817 | 288,187 | 256,529 | -7.7 | 10.9 | -11.0 | |
| 162 | Other OR therapeutic procedures on joints | 513,561 | 463,114 | 518,568 | 455,452 | -9.8 | 12.0 | -12.2 | |
| 164 | Other OR therapeutic procedures on musculoskeletal system | 43,797 | 43,683 | 55,635 | 49,358 | -0.3 | 27.4 | -11.3 | Inclusion of specialty hospitals: increase in 2019 after specialty hospitals were added to the NASS universe |
| 166 | Lumpectomy, quadrantectomy of breast | 317,702 | 317,525 | 331,735 | 291,853 | -0.1 | 4.5 | -12.0 | |
| 167 | Mastectomy | 79,764 | 86,585 | 94,411 | 92,734 | 8.6 | 9.0 | 1.8 | |
| 170 | Excision of skin lesion | 134,215 | 107,707 | -19.8 | Change to in-scope procedure criteria: in scope in 2019 because market share criterion was removed | ||||
| 171 | Suture of skin and subcutaneous tissue | 8,247 | 120,030 | 100,817 | -16.0 | Surgery Flag Software update: not in scope for 2018 because outpatient hospital share fell below threshold after reclassification of 6 CPT codes Change to in-scope procedure criteria: in scope in 2019 because market share criterion was removed |
|||
| 174 | Other non-OR therapeutic procedures on skin and breast | 19,753 | CCS for Services and Procedures update: not in scope for 2018 after all narrow procedures were reclassified from CCS 174 to CCS 175 | ||||||
| 175 | Other OR therapeutic procedures on skin and breast | 343,787 | 342,372 | 376,101 | 330,690 | -0.4 | 9.9 | -12.1 | |
| 225 | Conversion of cardiac rhythm | 136,840 | 149,475 | 169,206 | 158,750 | 9.2 | 13.2 | -6.2 | |
| 244 | Gastric bypass and volume reduction | 24,600 | 24,709 | 24,658 | 25,629 | 0.4 | -0.2 | 3.9 | |
| Abbreviations: CMS, Centers for Medicare & Medicaid Services; CPT, Current Procedural Terminology; GI, gastrointestinal; NASS, Nationwide Ambulatory Surgery Sample; OR, operating room; SEDD, State Emergency Department Databases a See CMS Hospital Outpatient Prospective Payment- Notice of Final Rulemaking (NFRM) with Comment Period (CMS-1678-FC), available at:https://www.govinfo.gov/content/pkg/FR-2017-11-13/pdf/2017-23932.pdf. Notes: Totals represent weighted estimates. CCS category totals are unduplicated, such that if two or more CPT codes on the same encounter record mapped to the same CCS category, the record was only counted once. Totals are missing if the CCS procedure category was not in scope for the NASS sample. Contributing reasons for changes over time are reported only for categories that were added to or removed from the NASS in-scope procedure list and for categories with year-to-year percentage change in volume greater than 20 percent. | |||||||||
1 The following States have at least one freestanding facility in the HCUP SASD: California, Florida, Illinois, Kentucky, Michigan, Missouri, North Carolina, Nevada, New York, Oklahoma, Oregon, Pennsylvania, South Carolina, Utah, and Wisconsin.
2 Agency for Healthcare Research and Quality. Surgery Flag Software for Services and Procedures. Healthcare Cost and Utilization Project (HCUP). Last modified May 31, 2022. www.hcup-us.ahrq.gov/toolssoftware/surgeryflags_svcproc/surgeryflagssvc_proc.jsp. Accessed September 22, 2022. For more information, reference the Surgery Flag Software for Services and Procedures User Guide, available at: www.hcup-us.ahrq.gov/toolssoftware/surgeryflags_svcproc/surgeryflagssvc_proc.jsp#user.
3 The Clinical Classifications Software for Services and Procedures (CCS-Services and Procedures) is HCUP software that provides a method for classifying CPT codes and Healthcare Common Procedure Coding System (HCPCS) codes into clinically meaningful procedure categories. More than 9,000 CPT/HCPCS codes and 6,000 HCPCS codes are collapsed into 244 clinically meaningful categories that may be more useful for presenting descriptive statistics than are individual CPT or HCPCS codes. For more information, visit www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp.
4 Clinical Classifications Software Refined (CCSR). Healthcare Cost and Utilization Project (HCUP). October 2021. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp. Accessed September 22, 2022.
5 Elixhauser Comorbidity Software Refined for ICD-10-CM Healthcare Cost and Utilization Project (HCUP). October 2021. Agency for Healthcare Research and Quality, Rockville, MD. www.hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp. Accessed September 22, 2022.
6 Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for Services and Procedures. Healthcare Cost and Utilization Project (HCUP). Last modified May 26, 2021. www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. Accessed September 22, 2022.
7 Agency for Healthcare Research and Quality. Surgery Flag Software for Services and Procedures. Healthcare Cost and Utilization Project (HCUP). Last modified May 31, 2022. www.hcup-us.ahrq.gov/toolssoftware/surgeryflags_svcproc/surgeryflagssvc_proc.jsp. Accessed September 22, 2022.
8 Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS) for Services and Procedures. Healthcare Cost and Utilization Project (HCUP). Last modified April 26, 2021. www.hcup-us.ahrq.gov/toolssoftware/ccs_svcsproc/ccssvcproc.jsp. Accessed September 16, 2021.
9 Percutaneous transluminal coronary angioplasty (PTCA) was included in earlier years of the NASS (2016 and 2017).
10 See the AHA "community hospital designation" at www.ahadataviewer.com/glossary.![]()
11 The AHA Annual Survey definition for outpatient surgery is as follows: Scheduled surgical services provided to patients who do not remain in the hospital overnight. The surgery may be performed in operating suites also used for inpatient surgery, specially designated surgical suites for outpatient surgery, or procedure rooms within an outpatient care facility. (American Hospital Association. TrendWatch Chartbook 2020 - Glossary. www.ahadata.com/system/files/media/file/2022/05/2020-AHA-Annual.pdf. ![]() Accessed September 22, 2022.)
Accessed September 22, 2022.)
12 The HCUP SASD contain a number of hospital-owned facilities performing major ambulatory surgeries that are not inpatient hospitals. In the NASS, these facilities are assigned the identifier of the hospital owner. Stratification, sampling, weighting, and reporting are performed using the hospital owner identifier and hospital characteristics.
13 Bed size categories were originally established for the development of the Nationwide Inpatient Sample (NIS). Cutoff points were chosen so that approximately one-third of the hospitals in each region, location, and teaching status combination would fall within each bed size category (small, medium, or large). For more information, reference the Introduction to the NIS, available at www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
14 Hospital service type was not used as a stratum because of its weaker predictive power in the predictive models and the small number of children's hospitals in the sample.
15 The sampling fraction is defined as (number units in sample)/(number units in universe). The overall sampling fraction for the 2020 universe of hospitals and sampling frame is (2,899/4,352) = 0.67.
16 The ownership category was chosen for collapsing because it had lower explanatory power in the predictive models than did bed size or location and teaching status. Census region was considered as an essential stratum to include in the design.
17 Carlson BL, Johnson AE, Cohen SB. An evaluation of the use of personal computers for variance estimation with complex survey data. J Off Statistics. 1993;9(4):795-814.
| Internet Citation: 2020 Introduction to the NASS. Healthcare Cost and Utilization Project (HCUP). November 2022. Agency for Healthcare Research and Quality, Rockville, MD. hcup-us.ahrq.gov/db/nation/nass/NASS_Introduction_2020.jsp. |
| Are you having problems viewing or printing pages on this website? |
| If you have comments, suggestions, and/or questions, please contact hcup@ahrq.gov. |
| If you are experiencing issues related to Section 508 accessibility of information on this website, please contact hcup@ahrq.gov. |
| Privacy Notice, Viewers & Players |
| Last modified 11/10/22 |